
Referrals

Support for Care Partners and Your Patients
Tidewell Hospice is here to support you and your patients diagnosed with a life-limiting illness wherever they call home. We partner with you and your patients and their families for the management of pain and symptoms. The benefits of our hospice care can result in fewer hospital stays or emergency room visits, increased patient coping skills, improved quality of life and some patients even live longer. In addition, we offer specialized care for end-stage heart failure and COPD patients care for their diagnoses.
General Hospice Admission Criteria
In order to meet eligibility requirements, a physician must reasonably believe the patient's prognosis to be six months or less if the disease runs its normal course. Each patient is unique in his or her response to disease processes, and the specifications listed below only serve as a guide to support an physician's opinion the patient may be hospice appropriate.
Call Tidewell Hospice at (941) 894-1777 to discuss hospice eligibility and for any further questions.
Cancer Patients
Patients must meet all of the following criteria:
- Clinical findings of malignancy with widespread, aggressive or progressive disease as evidenced by increasing symptoms, worsening lab values and/or evidence of metastatic disease
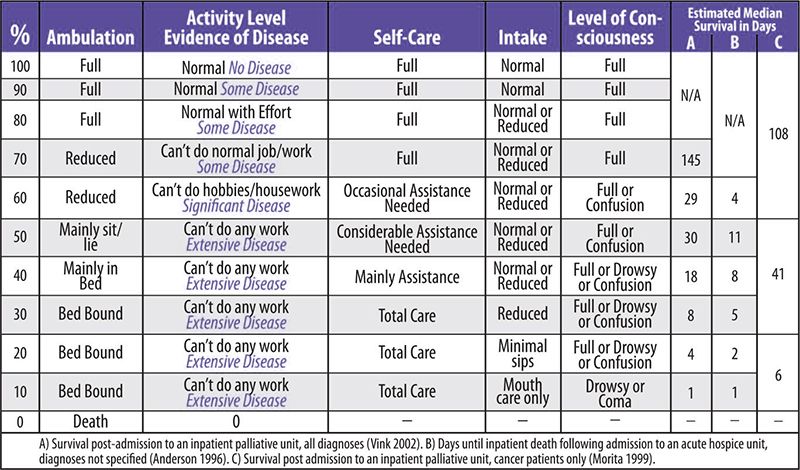
- Palliative performance scale (PPS) ≤ 70%
- Refuses further life-prolonging therapy OR continues to decline in spite of definitive therapy
Supporting documentation includes:
- Clinical findings of malignancy with widespread, aggressive or progressive disease as evidenced by increasing symptoms, worsening lab values and/or evidence of metastatic disease
- Palliative performance scale (PPS) ≤ 70%
- Refuses further life-prolonging therapy OR continues to decline in spite of definitive therapy
Cardiac Patients
The patient has 1 and either 2 or 3.
CHF with NYHA Class IV symptoms & both:
Significant symptoms at rest
- Inability to carry out even minimal physical activity without dyspnea or angina
- Patient is optimally treated (diuretics, vasodilators, ACEI, or hydralazine and nitrates)
- The patient has angina pectoris at rest, resistant to standard nitrate therapy, and is either not a candidate for/or has declined invasive procedures.
Supporting documentation includes:
EF ≤ 20%, treatment-resistant symptomatic dysrhythmias History of cardiac-related syncope CVA 2/2 cardiac embolism History of cardiac resuscitation
COPD and Pulmonary Patients
Severe chronic lung disease as documented by 1, 2 and 3.
- The patient has all of the following:
- Disabling dyspnea at rest
- Little if no response to bronchodilators
- Decreased functional capacity (bed to chair existence, fatigue and cough)
AND
- Progression of disease as evidenced by a recent history of increasing physicians' office, home or ED visits and or hospitalizations for pulmonary infection and/or respiratory failure
AND
- Documentation within the past 3 months ≥1:
- Hypoxemia at rest on room air (p02 < 55 mmHg by ABG) or oxygen saturation < 88%
- Hypercapnia evidenced by pC02 > 50 mmHg
Supporting documentation includes:
- Cor pulmonale and right heart failure.
- Unintentional progressive weight loss
Alzheimer’s and Dementia Patients
The patient must have both:
- Stage 7C or beyond according to the FAST Scale
- One or more of the following conditions in the past 12 months:
- Aspiration pneumonia
- Pyelonephritis
- Septicemia
- Multiple pressure ulcers (stage 3-4)
- Recurrent fever
- Other significant condition that suggests a limited prognosis
- Inability to maintain sufficient fluid and calorie intake in the past 6 months (10% weight loss or albumin < 2.5 gm/dl)
Dementia Functional Assessment Scale Tool (FAST)
- No difficulty either subjectively or objectively.
- Complains of forgetting location of objects. Subjective work difficulties.
- Decreased job functioning evident to co-workers. Difficulty in traveling to new locations. Decreased organizational capacity.*
- Decreases ability to perform complex task, (e.g., planning dinner for guests, handling personal finances e.g. forgetting to pay bill, etc.)
- Requires assistance in choosing proper clothing to wear for the day, season or occasion, (e.g. pt may wear the same clothing repeatedly, unless supervised.*
- Occasionally or more frequently over the past weeks. * for the following
- Improperly putting on clothes without assistance or cueing.
- Unable to bathe properly (not able to choose proper water temp)
- Inability to handle mechanics of toileting (e.g., forget to flush the toilet does not wipe properly or dispose of toilet tissue)
- Urinary incontinence
- Fecal incontinence
- Ability to speak limited to approximately < 6 intelligible different words in the course of an average day or in the course of an intensive interview.
- Speech ability is limited to the use of a single intelligible word in an average day or in the course of an intensive interview
- Ambulatory ability is lost (cannot walk without personal assistance.)
- Cannot sit up without assistance (e.g., the individual will fall over if there are not lateral rests [arms] on the chair.)
- Loss of ability to smile
- Loss of ability to hold up head independently.
* Scored primarily on information obtained from a knowledgeable informant.
HIV/AIDS Patients
The patient has either 1A or 1B and 2 and 3.
1A. CD4+ < 25 cells/mcL
OR
1B. Viral load > 100,000
AND
2. At least one:
- CNS lymphoma
- Untreated or refractory wasting (loss of > 33% lean body mass)
- MAC bacteremia
- Progressive multifocal leukoencephalopathy
- Systemic lymphoma
- Visceral KS
- Renal failure no HD
- Cryptosporidium infection
- Refractory toxoplasmosis
AND
3. Palliative performance scale of < 50%
Liver Disease Patients
The patient has both:
- End-stage liver disease as demonstrated by A or B & C:
- PT> 5 sec
OR
- INR > 1.5
AND
- Serum albumin <2.5 gm / dl
AND
One or more of the following conditions:
- Refractory ascites
- History of spontaneous bacterial peritonitis
- Hepatorenal syndrome
- Refractory hepatic encephalopathy
- History of recurrent variceal bleeding
Supporting Documents include:
- Progressive malnutrition
- Muscle wasting with decreased strength
- Ongoing alcoholism (> 80 gm ethanol/day)
- Hepatocellular CA HBsAg positive
- Hep. C refractory to treatment
Neurologic Disease Patients
Criteria are very similar for chronic degenerative conditions such as ALS, Parkinson's, muscular dystrophy, myasthenia gravis or multiple sclerosis
The patient must meet at least one of the following criteria (1 or 2A or 2B):
- Critically-impaired breathing capacity, with all:
- Dyspnea at rest
- Vital capacity < 30%
- Need O2 at rest
- Patient refuses artificial ventilation
OR
- Rapid disease progression any of the following and either A or B below:
- Independent ambulation to wheelchair- or bed-bound status
- Normal to barely intelligible or unintelligible speech
- Normal to pureed diet
- Independence in most ADLs to needing major assistance in all ADLs
AND
- Critical nutritional impairment demonstrated by all of the following in the preceding 12 months:
- Oral intake of nutrients and fluids insufficient to sustain life
- Continuing weight loss
- Dehydration or hypovolemia
- Absence of artificial feeding methods
OR
2. Life-threatening complications in the past 12 months as demonstrated by ≥1:
- Recurrent aspiration pneumonia, pyelonephritis, sepsis
- Recurrent fever, Stage 3 or 4 pressure ulcer(s)
Renal Disease Patients
Patient has 1, 2 and 3.
- The patient is not seeking dialysis or renal transplant
- Creatinine clearance* is < 10 cc/min (<15 for diabetics)
- Serum creatinine > 8.0 mg/dl (> 6.0 mg/dl for diabetics)
Supporting documentation for chronic renal failure includes:
- Uremia
- Oliguria (urine output < 400 cc in 24 hours)
- Intractable hyperkalemia (> 7.0)
- Uremic pericarditis
- Hepatorenal syndrome
- Intractable fluid overload
Supporting documentation for acute renal failure includes:
- Mechanical ventilation
- Malignancy (other organ system)
- Chronic lung disease
- Advanced cardiac disease
- Advanced liver disease
*Values adjusted for older patients or patients with comorbidities
Stroke or Coma Patients
Patient has both.
- Poor functional status palliative performance scale ≤ 40%
- Poor nutritional status with inability to maintain sufficient fluid and calorie intake with ≥ 1 of the following:
- ≥ 10% weight loss in past 6 months
- ≥ 7.5% weight loss in past 3 months
- Serum albumin < 2.5 gm/dl
- Current history of pulmonary aspiration without effective response to speech therapy interventions to improve dysphagia and decrease aspiration events
Supporting documentation includes:
Coma (any etiology) with 3 of the following on the third day of coma:
- Abnormal brain stem response
- Absent verbal responses
- Absent withdrawal response to pain
- Serum creatinine > 1.5 gm/dl
